What Can You Do About Fallen Arches?
Overview

Fallen arches or flat feet is a condition in which the arch or instep of the foot collapses and comes in contact with the ground. In some individuals, this arch never develops while they are growing. Flat feet (also called pes planus or fallen arches) is a formal reference to a medical condition in which the arch of the foot collapses, with the entire sole of the foot coming into complete or near-complete contact with the ground. In some individuals (an estimated 20-30% of the general population) the arch simply never develops in one foot (unilaterally) or both feet (bilaterally).
Causes
Fallen arches can be the result of other conditions such as overuse, stretching or tearing of the posterior tibial tendon (which attaches to a bone in the foot and runs up the calf of the lower leg at a tension which pulls up the arch) which reduces its ability to maintain tension in the tendon. Whether or not the condition is caused by overpronation, this is the likely outcome for runners, whose arches are no longer strong enough to take the constant strain of bearing the body?s weight on impact, causing joint, postural and muscular problems.
Symptoms
Pain and stiffness of the medial arch or anywhere along the mid-portion of the foot. Associated discomfort within and near the ankle joint. The knees, hips, and lower back may be the primary source of discomfort. Feet may often feel tired and achy. Painful shin splints may develop with activity. Gait may be awkward.
Diagnosis
Flat feet are easy to identify while standing or walking. When someone with flat feet stands, their inner foot or arch flattens and their foot may roll over to the inner side. This is known as overpronation. To see whether your foot overpronates, stand on tiptoes or push your big toe back as far as possible. If the arch of your foot doesn't appear, your foot is likely to overpronate when you walk or run. It can be difficult to tell whether a child has flat feet because their arches may not fully develop until they're 10 years of age.
What causes pes planus?
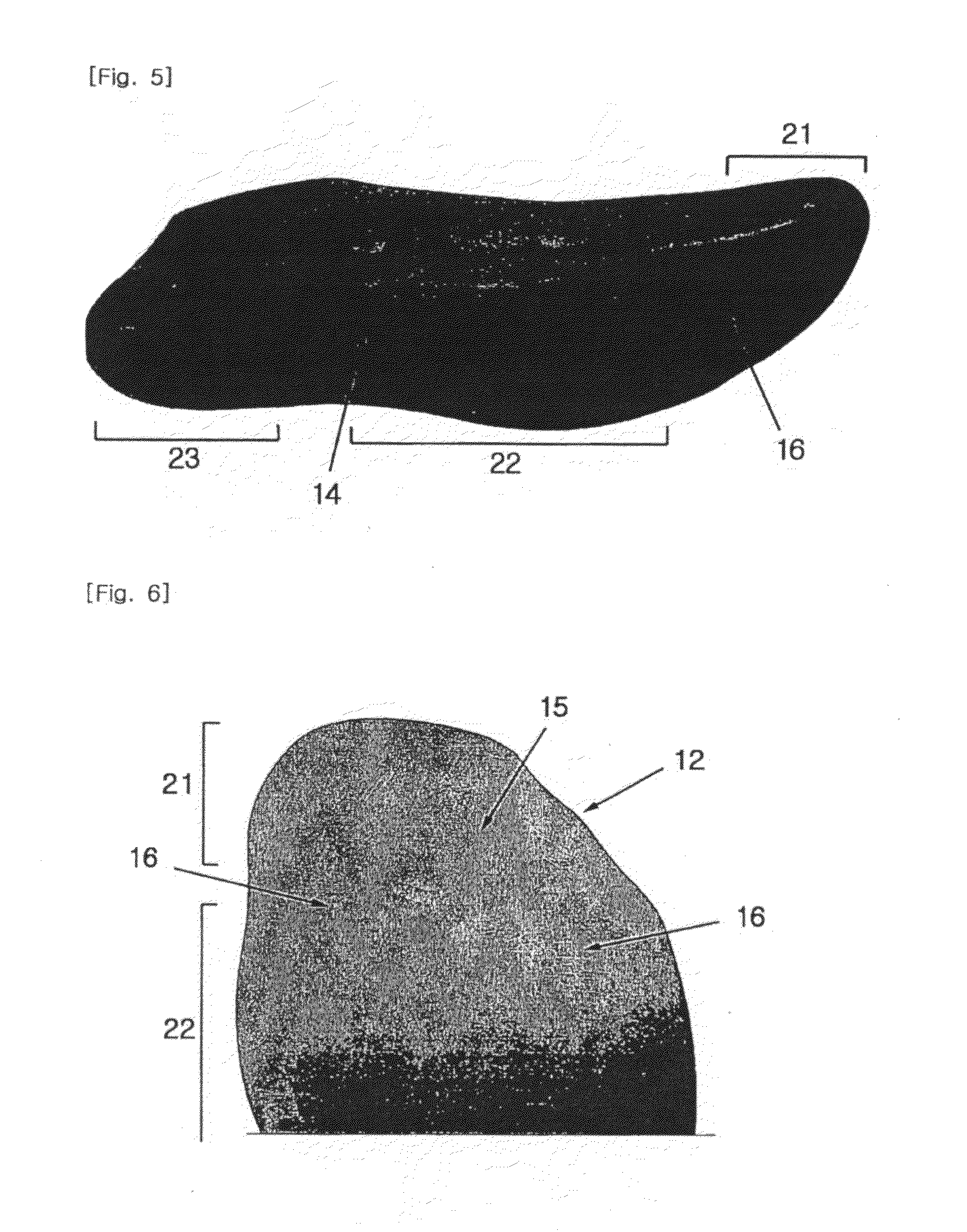
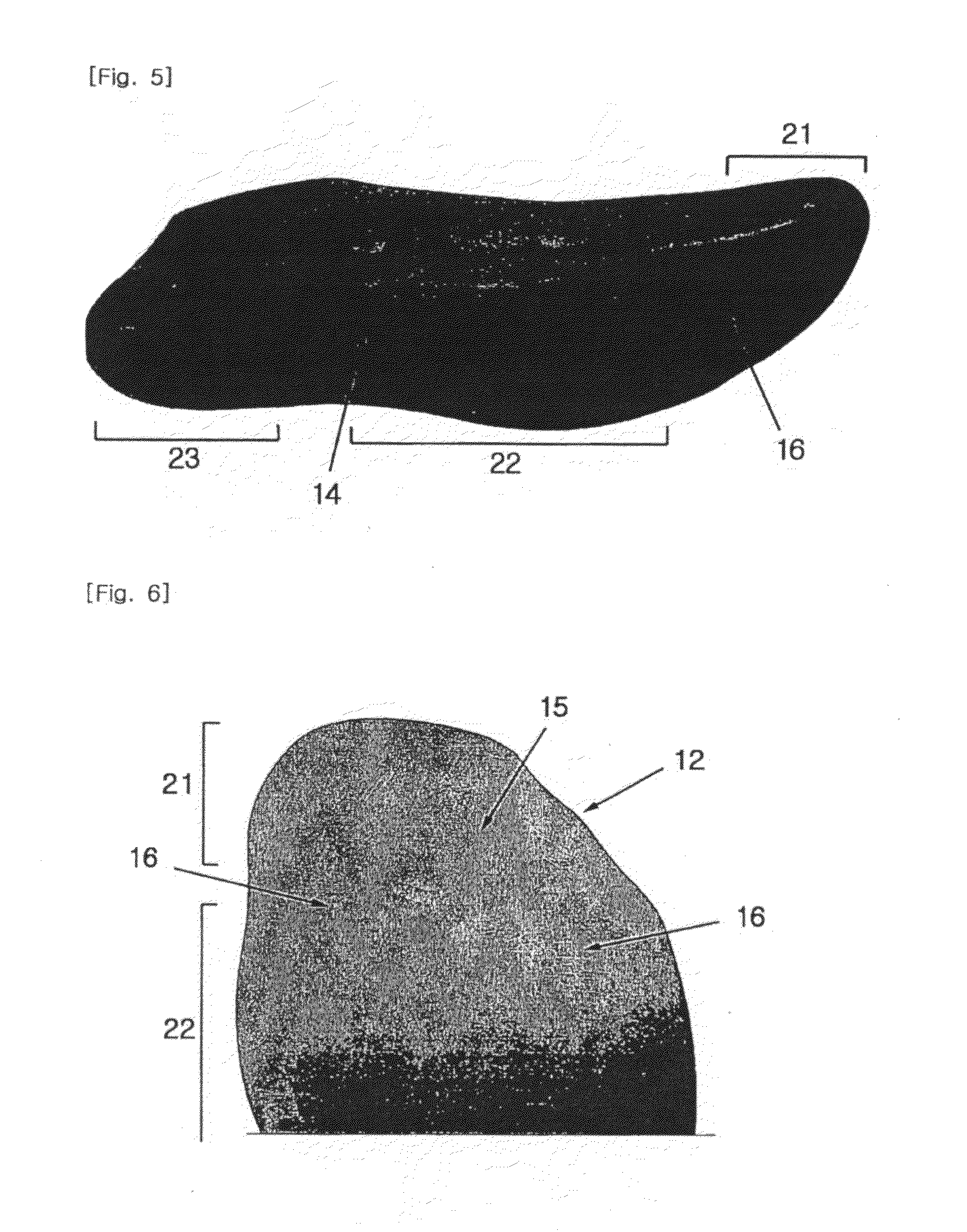
Non Surgical Treatment
What we want to do is support the arch and maintain it in that curved position. So what you want is to bring the foot into a position where you hold and support the arch so you can get that correct heel-midfoot-big toe contact. You would achieve that with a level of arch support. People will take different levels of support, if you?re somebody who has movement in your arch, a strong level of support will hold and maintain you whereas if you?re someone whose arch has collapsed it could need more support and a level of correction built into the support to realign you. If you think of it, when your arch drops, it affects your foot but it also has a biomechanical effect on the rest of the body. But nothing that can?t be solved.
Surgical Treatment

Surgical correction is dependent on the severity of symptoms and the stage of deformity. The goals of surgery are to create a more functional and stable foot. There are multiple procedures available to the surgeon and it may take several to correct a flatfoot deformity. Stage one deformities usually respond to conservative or non-surgical therapy such as anti-inflammatory medication, casting, functional orthotics or a foot ankle orthosis called a Richie Brace. If these modalities are unsuccessful surgery is warranted. Usually surgical treatment begins with removal of inflammatory tissue and repair of the posterior tibial tendon. A tendon transfer is performed if the posterior tibial muscle is weak or the tendon is badly damaged. The most commonly used tendon is the flexor digitorum longus tendon. This tendon flexes or moves the lesser toes downward. The flexor digitorum longus tendon is utilized due to its close proximity to the posterior tibial tendon and because there are minimal side effects with its loss. The remainder of the tendon is sutured to the flexor hallucis longus tendon that flexes the big toe so that little function is loss. Stage two deformities are less responsive to conservative therapies that can be effective in mild deformities. Bone procedures are necessary at this stage in order to recreate the arch and stabilize the foot. These procedures include isolated fusion procedures, bone grafts, and/or the repositioning of bones through cuts called osteotomies. The realigned bones are generally held in place with screws, pins, plates, or staples while the bone heals. A tendon transfer may or may not be utilized depending on the condition of the posterior tibial tendon. Stage three deformities are better treated with surgical correction, in healthy patients. Patients that are unable to tolerate surgery or the prolonged healing period are better served with either arch supports known as orthotics or bracing such as the Richie Brace. Surgical correction at this stage usually requires fusion procedures such as a triple or double arthrodesis. This involves fusing the two or three major bones in the back of the foot together with screws or pins. The most common joints fused together are the subtalar joint, talonavicular joint, and the calcaneocuboid joint. By fusing the bones together the surgeon is able to correct structural deformity and alleviate arthritic pain. Tendon transfer procedures are usually not beneficial at this stage. Stage four deformities are treated similarly but with the addition of fusing the ankle joint.
Prevention
Going barefoot, particularly over terrain such as a beach where muscles are given a good workout, is good for all but the most extremely flatfooted, or those with certain related conditions such as plantar fasciitis. Ligament laxity is also among the factors known to be associated with flat feet. One medical study in India with a large sample size of children who had grown up wearing shoes and others going barefoot found that the longitudinal arches of the bare footers were generally strongest and highest as a group, and that flat feet were less common in children who had grown up wearing sandals or slippers than among those who had worn closed-toe shoes. Focusing on the influence of footwear on the prevalence of pes planus, the cross-sectional study performed on children noted that wearing shoes throughout early childhood can be detrimental to the development of a normal or a high medial longitudinal arch. The vulnerability for flat foot among shoe-wearing children increases if the child has an associated ligament laxity condition. The results of the study suggest that children be encouraged to play barefooted on various surfaces of terrain and that slippers and sandals are less harmful compared to closed-toe shoes. It appeared that closed-toe shoes greatly inhibited the development of the arch of the foot more so than slippers or sandals. This conclusion may be a result of the notion that intrinsic muscle activity of the arch is required to prevent slippers and sandals from falling off the child?s foot.
After Care
Patients may go home the day of surgery or they may require an overnight hospital stay. The leg will be placed in a splint or cast and should be kept elevated for the first two weeks. At that point, sutures are removed. A new cast or a removable boot is then placed. It is important that patients do not put any weight on the corrected foot for six to eight weeks following the operation. Patients may begin bearing weight at eight weeks and usually progress to full weightbearing by 10 to 12 weeks. For some patients, weightbearing requires additional time. After 12 weeks, patients commonly can transition to wearing a shoe. Inserts and ankle braces are often used. Physical therapy may be recommended. There are complications that relate to surgery in general. These include the risks associated with anesthesia, infection, damage to nerves and blood vessels, and bleeding or blood clots. Complications following flatfoot surgery may include wound breakdown or nonunion (incomplete healing of the bones). These complications often can be prevented with proper wound care and rehabilitation. Occasionally, patients may notice some discomfort due to prominent hardware. Removal of hardware can be done at a later time if this is an issue. The overall complication rates for flatfoot surgery are low.
Fallen arches or flat feet is a condition in which the arch or instep of the foot collapses and comes in contact with the ground. In some individuals, this arch never develops while they are growing. Flat feet (also called pes planus or fallen arches) is a formal reference to a medical condition in which the arch of the foot collapses, with the entire sole of the foot coming into complete or near-complete contact with the ground. In some individuals (an estimated 20-30% of the general population) the arch simply never develops in one foot (unilaterally) or both feet (bilaterally).
Causes
Fallen arches can be the result of other conditions such as overuse, stretching or tearing of the posterior tibial tendon (which attaches to a bone in the foot and runs up the calf of the lower leg at a tension which pulls up the arch) which reduces its ability to maintain tension in the tendon. Whether or not the condition is caused by overpronation, this is the likely outcome for runners, whose arches are no longer strong enough to take the constant strain of bearing the body?s weight on impact, causing joint, postural and muscular problems.
Symptoms
Pain and stiffness of the medial arch or anywhere along the mid-portion of the foot. Associated discomfort within and near the ankle joint. The knees, hips, and lower back may be the primary source of discomfort. Feet may often feel tired and achy. Painful shin splints may develop with activity. Gait may be awkward.
Diagnosis
Flat feet are easy to identify while standing or walking. When someone with flat feet stands, their inner foot or arch flattens and their foot may roll over to the inner side. This is known as overpronation. To see whether your foot overpronates, stand on tiptoes or push your big toe back as far as possible. If the arch of your foot doesn't appear, your foot is likely to overpronate when you walk or run. It can be difficult to tell whether a child has flat feet because their arches may not fully develop until they're 10 years of age.
What causes pes planus?
Non Surgical Treatment
What we want to do is support the arch and maintain it in that curved position. So what you want is to bring the foot into a position where you hold and support the arch so you can get that correct heel-midfoot-big toe contact. You would achieve that with a level of arch support. People will take different levels of support, if you?re somebody who has movement in your arch, a strong level of support will hold and maintain you whereas if you?re someone whose arch has collapsed it could need more support and a level of correction built into the support to realign you. If you think of it, when your arch drops, it affects your foot but it also has a biomechanical effect on the rest of the body. But nothing that can?t be solved.
Surgical Treatment

Surgical correction is dependent on the severity of symptoms and the stage of deformity. The goals of surgery are to create a more functional and stable foot. There are multiple procedures available to the surgeon and it may take several to correct a flatfoot deformity. Stage one deformities usually respond to conservative or non-surgical therapy such as anti-inflammatory medication, casting, functional orthotics or a foot ankle orthosis called a Richie Brace. If these modalities are unsuccessful surgery is warranted. Usually surgical treatment begins with removal of inflammatory tissue and repair of the posterior tibial tendon. A tendon transfer is performed if the posterior tibial muscle is weak or the tendon is badly damaged. The most commonly used tendon is the flexor digitorum longus tendon. This tendon flexes or moves the lesser toes downward. The flexor digitorum longus tendon is utilized due to its close proximity to the posterior tibial tendon and because there are minimal side effects with its loss. The remainder of the tendon is sutured to the flexor hallucis longus tendon that flexes the big toe so that little function is loss. Stage two deformities are less responsive to conservative therapies that can be effective in mild deformities. Bone procedures are necessary at this stage in order to recreate the arch and stabilize the foot. These procedures include isolated fusion procedures, bone grafts, and/or the repositioning of bones through cuts called osteotomies. The realigned bones are generally held in place with screws, pins, plates, or staples while the bone heals. A tendon transfer may or may not be utilized depending on the condition of the posterior tibial tendon. Stage three deformities are better treated with surgical correction, in healthy patients. Patients that are unable to tolerate surgery or the prolonged healing period are better served with either arch supports known as orthotics or bracing such as the Richie Brace. Surgical correction at this stage usually requires fusion procedures such as a triple or double arthrodesis. This involves fusing the two or three major bones in the back of the foot together with screws or pins. The most common joints fused together are the subtalar joint, talonavicular joint, and the calcaneocuboid joint. By fusing the bones together the surgeon is able to correct structural deformity and alleviate arthritic pain. Tendon transfer procedures are usually not beneficial at this stage. Stage four deformities are treated similarly but with the addition of fusing the ankle joint.
Prevention
Going barefoot, particularly over terrain such as a beach where muscles are given a good workout, is good for all but the most extremely flatfooted, or those with certain related conditions such as plantar fasciitis. Ligament laxity is also among the factors known to be associated with flat feet. One medical study in India with a large sample size of children who had grown up wearing shoes and others going barefoot found that the longitudinal arches of the bare footers were generally strongest and highest as a group, and that flat feet were less common in children who had grown up wearing sandals or slippers than among those who had worn closed-toe shoes. Focusing on the influence of footwear on the prevalence of pes planus, the cross-sectional study performed on children noted that wearing shoes throughout early childhood can be detrimental to the development of a normal or a high medial longitudinal arch. The vulnerability for flat foot among shoe-wearing children increases if the child has an associated ligament laxity condition. The results of the study suggest that children be encouraged to play barefooted on various surfaces of terrain and that slippers and sandals are less harmful compared to closed-toe shoes. It appeared that closed-toe shoes greatly inhibited the development of the arch of the foot more so than slippers or sandals. This conclusion may be a result of the notion that intrinsic muscle activity of the arch is required to prevent slippers and sandals from falling off the child?s foot.
After Care
Patients may go home the day of surgery or they may require an overnight hospital stay. The leg will be placed in a splint or cast and should be kept elevated for the first two weeks. At that point, sutures are removed. A new cast or a removable boot is then placed. It is important that patients do not put any weight on the corrected foot for six to eight weeks following the operation. Patients may begin bearing weight at eight weeks and usually progress to full weightbearing by 10 to 12 weeks. For some patients, weightbearing requires additional time. After 12 weeks, patients commonly can transition to wearing a shoe. Inserts and ankle braces are often used. Physical therapy may be recommended. There are complications that relate to surgery in general. These include the risks associated with anesthesia, infection, damage to nerves and blood vessels, and bleeding or blood clots. Complications following flatfoot surgery may include wound breakdown or nonunion (incomplete healing of the bones). These complications often can be prevented with proper wound care and rehabilitation. Occasionally, patients may notice some discomfort due to prominent hardware. Removal of hardware can be done at a later time if this is an issue. The overall complication rates for flatfoot surgery are low.
Leg Length Discrepancy Subsequent To Knee Surgery
Overview
Leg length discrepancy (LLD) or Lower limb discrepancy is a condition of unequal lengths of the lower limbs. The discrepancy may be in the femur, or tibia, or both. In some conditions, the whole side is affected, including the upper limbs. However, it is the discrepancy of the lower limbs that causes problems with ambulation, and the focus of this discussion will be about lower limb discrepancy.
Causes
From an anatomical stand point, the LLD could have been from hereditary, broken bones, diseases and joint replacements. Functional LLD can be from over pronating, knee deformities, tight calves and hamstrings, weak IT band, curvature in the spine and many other such muscular/skeletal issues.
Symptoms
Children whose limbs vary in length often experience difficulty using their arms or legs. They might have difficulty walking or using both arms to engage in everyday activities.
Diagnosis
Limb length discrepancy can be measured by a physician during a physical examination and through X-rays. Usually, the physician measures the level of the hips when the child is standing barefoot. A series of measured wooden blocks may be placed under the short leg until the hips are level. If the physician believes a more precise measurement is needed, he or she may use X-rays. In growing children, a physician may repeat the physical examination and X-rays every six months to a year to see if the limb length discrepancy has increased or remained unchanged. A limb length discrepancy may be detected on a screening examination for curvature of the spine (scoliosis). But limb length discrepancy does not cause scoliosis.
Non Surgical Treatment
Treatment depends on the amount and cause of the leg length discrepancy as well as the age of your child. Typically, if the difference is less than 2 cm we don?t recommend immediate treatment. We may recommend that your child wear a heel lift in one shoe to make walking and running more comfortable. If the leg length discrepancy is more significant, your doctor may recommend surgery to shorten or lengthen a leg. The procedure used most often to shorten a leg is called epiphysiodesis.

how we can increase our height?
Surgical Treatment
For discrepancies over five centimeters, more aggressive surgical procedures-specifically leg lengthening procedures-are typically required. The specifics of this operative procedure are beyond the scope of this informational page, but your child's physician will be able to discuss the details in reference to your child's specific problems when considered appropriate.
Leg length discrepancy (LLD) or Lower limb discrepancy is a condition of unequal lengths of the lower limbs. The discrepancy may be in the femur, or tibia, or both. In some conditions, the whole side is affected, including the upper limbs. However, it is the discrepancy of the lower limbs that causes problems with ambulation, and the focus of this discussion will be about lower limb discrepancy.

Causes
From an anatomical stand point, the LLD could have been from hereditary, broken bones, diseases and joint replacements. Functional LLD can be from over pronating, knee deformities, tight calves and hamstrings, weak IT band, curvature in the spine and many other such muscular/skeletal issues.
Symptoms
Children whose limbs vary in length often experience difficulty using their arms or legs. They might have difficulty walking or using both arms to engage in everyday activities.
Diagnosis
Limb length discrepancy can be measured by a physician during a physical examination and through X-rays. Usually, the physician measures the level of the hips when the child is standing barefoot. A series of measured wooden blocks may be placed under the short leg until the hips are level. If the physician believes a more precise measurement is needed, he or she may use X-rays. In growing children, a physician may repeat the physical examination and X-rays every six months to a year to see if the limb length discrepancy has increased or remained unchanged. A limb length discrepancy may be detected on a screening examination for curvature of the spine (scoliosis). But limb length discrepancy does not cause scoliosis.
Non Surgical Treatment
Treatment depends on the amount and cause of the leg length discrepancy as well as the age of your child. Typically, if the difference is less than 2 cm we don?t recommend immediate treatment. We may recommend that your child wear a heel lift in one shoe to make walking and running more comfortable. If the leg length discrepancy is more significant, your doctor may recommend surgery to shorten or lengthen a leg. The procedure used most often to shorten a leg is called epiphysiodesis.

how we can increase our height?
Surgical Treatment
For discrepancies over five centimeters, more aggressive surgical procedures-specifically leg lengthening procedures-are typically required. The specifics of this operative procedure are beyond the scope of this informational page, but your child's physician will be able to discuss the details in reference to your child's specific problems when considered appropriate.
What Are The Causes Of Heel Painfulness
Overview

One of the most common foot problems seen by physicians is heel pain. Heel pain that occurs in adult patients is most commonly caused by a condition known as plantar fasciitis. This condition is sometimes also known as a heel spur. Heel pain can also be caused by other factors, such as stress fracture, tendinitis, arthritis, nerve entrapment, cyst in the heel bone.
Causes
Many things can cause heel pain. Most commonly seen at our Troy, MI office are heel spurs, which are small growths on the heel bone. Heel pain can be caused from heavy activities and increased weight that put extra pressure on feet. Dr. Weinert often treats heel pain in athletes, runners and women who are pregnant. There are other cases where Dr. Weinert has related a patient?s heel pain to arthritis, stress fractures, fractures, bone tumors, cysts, achilles tendonitis and Haglund's deformity. The main cause of heel pain is usually a biomechanical problem in the foot and it?s, in a nutshell, having a foot out of alignment. There are numerous conditions. One of the most prevalent is called talotarsal dislocation syndrome. What that is in lay terms is you?ve just got a misalignment of your ankle on your heel and as you bear weight you?re getting a collapse of the ankle on the heel causing the foot to be out of alignment. So the plantar fascia, bones, joints, and ligaments receive constant stress. This stress occurs at the point where the plantar fascia (the major tissue that connects your toes to your heel) meets the heel. Many patients explain the pain as being in the middle of the inside of the heel. As a patient bears weight, they get the collapse of the foot and that ligament pulls. And if you think of a rubber band constantly getting pulled on that area of the insertion on the heel, you eventually start getting some micro tears in that ligament and causing inflammation and pain specifically right there in middle area of the heel. Plantar fasciitis is also a common source of heel pain. The plantar fascia, a band of tissue that runs from your heel to your toes, can become strained and inflamed due to overuse and wear and tear. This band of tissue can only withstand so much pressure and when it gives way, the pain can be severe and requires immediate and effective treatment.
Symptoms
Both heel pain and heel spurs are frequently associated with an inflammation of the long band of tissue that connects the heel and the ball of the foot. The inflammation of this arch area is called plantar fasciitis. The inflammation maybe aggravated by shoes that lack appropriate support and by the chronic irritation that sometimes accompanies an athletic lifestyle. Achilles Tendinopathy, Pain and inflammation of the tendon at the back of the heel that connects the calf muscle to the foot. Sever?s, Often found in children between the ages of 8 - 13 years and is an inflammation of the calcaneal epiphyseal plate (growth plate) in the back of the heel. Bursitis, An inflamed bursa is a small irritated sack of fluid at the back of the heel. Other types of heel pain include soft tissue growths, Haglunds deformity (bone enlargement at the back of the heel), bruises or stress fractures and possible nerve entrapment.
Diagnosis
A biomechanical exam by your podiatrist will help reveal these abnormalities and in turn resolve the cause of plantar fasciitis. By addressing this cause, the patient can be offered a podiatric long-term solution to his problem.
Non Surgical Treatment
Recommended treatments, heel Spurs: cushioning for the heel is of little value. Your chiropodist/podiatrist may initially apply padding and strapping to alter the direction of stretch of the ligament. This is often successful at reducing the tenderness in the short term. Your chiropodist/podiatrist may suggest a course of deep heat therapy to stimulate the healing processes, allowing damage to respond and heal faster. In the long term, your chiropodist/podiatrist may prescribe special insoles (orthoses) to help the feet to function more effectively, thereby reducing strain on the ligaments and making any recurrence less likely. If pain from heel spurs continues, you may be referred to your GP who can prescribe an oral non-steroidal anti-inflammatory. Alternatively, localised hydrocortisone injection treatment may be given by your GP or an appropriate chiropodist/podiatrist. If pain persists, surgery may be considered. Heel Bursitis: in most cases, attention to the cause of any rubbing, and appropriate padding and strapping by your chiropodist/podiatrist will allow the inflammation to settle. If infection is present, your chiropodist/podiatrist will refer you to your GP for antibiotics. Heel Bumps: adjustments to footwear is often enough to make them comfortable. A leather heel counter and wearing boots may help. However, if pain persists, surgery may be necessary.
Surgical Treatment
Extracorporeal shockwave therapy (EST) is a fairly new type of non-invasive treatment. Non-invasive means it does not involve making cuts into your body. EST involves using a device to deliver high-energy soundwaves into your heel. The soundwaves can sometimes cause pain, so a local anaesthetic may be used to numb your heel. It is claimed that EST works in two ways. It is thought to have a "numbing" effect on the nerves that transmit pain signals to your brain, help stimulate and speed up the healing process. However, these claims have not yet been definitively proven. The National Institute for Health and Care Excellence (NICE) has issued guidance about the use of EST for treating plantar fasciitis. NICE states there are no concerns over the safety of EST, but there are uncertainties about how effective the procedure is for treating heel pain. Some studies have reported that EST is more effective than surgery and other non-surgical treatments, while other studies found the procedure to be no better than a placebo (sham treatment).
no foot pain
Prevention

Before you get out of bed in the morning, and then periodically throughout the day, do the following exercises to increase flexibility and ease pain. Slowly flex your foot and toes to stretch the tissue on the bottom of your sore foot. Hold the stretch for 10 counts. Relax and repeat. Do gentle ankle rolls to keep the tissues around the ankle and on the back of the heel flexible. Sit on the edge of your bed and roll your foot back and forth over a tennis ball.

One of the most common foot problems seen by physicians is heel pain. Heel pain that occurs in adult patients is most commonly caused by a condition known as plantar fasciitis. This condition is sometimes also known as a heel spur. Heel pain can also be caused by other factors, such as stress fracture, tendinitis, arthritis, nerve entrapment, cyst in the heel bone.
Causes
Many things can cause heel pain. Most commonly seen at our Troy, MI office are heel spurs, which are small growths on the heel bone. Heel pain can be caused from heavy activities and increased weight that put extra pressure on feet. Dr. Weinert often treats heel pain in athletes, runners and women who are pregnant. There are other cases where Dr. Weinert has related a patient?s heel pain to arthritis, stress fractures, fractures, bone tumors, cysts, achilles tendonitis and Haglund's deformity. The main cause of heel pain is usually a biomechanical problem in the foot and it?s, in a nutshell, having a foot out of alignment. There are numerous conditions. One of the most prevalent is called talotarsal dislocation syndrome. What that is in lay terms is you?ve just got a misalignment of your ankle on your heel and as you bear weight you?re getting a collapse of the ankle on the heel causing the foot to be out of alignment. So the plantar fascia, bones, joints, and ligaments receive constant stress. This stress occurs at the point where the plantar fascia (the major tissue that connects your toes to your heel) meets the heel. Many patients explain the pain as being in the middle of the inside of the heel. As a patient bears weight, they get the collapse of the foot and that ligament pulls. And if you think of a rubber band constantly getting pulled on that area of the insertion on the heel, you eventually start getting some micro tears in that ligament and causing inflammation and pain specifically right there in middle area of the heel. Plantar fasciitis is also a common source of heel pain. The plantar fascia, a band of tissue that runs from your heel to your toes, can become strained and inflamed due to overuse and wear and tear. This band of tissue can only withstand so much pressure and when it gives way, the pain can be severe and requires immediate and effective treatment.
Symptoms
Both heel pain and heel spurs are frequently associated with an inflammation of the long band of tissue that connects the heel and the ball of the foot. The inflammation of this arch area is called plantar fasciitis. The inflammation maybe aggravated by shoes that lack appropriate support and by the chronic irritation that sometimes accompanies an athletic lifestyle. Achilles Tendinopathy, Pain and inflammation of the tendon at the back of the heel that connects the calf muscle to the foot. Sever?s, Often found in children between the ages of 8 - 13 years and is an inflammation of the calcaneal epiphyseal plate (growth plate) in the back of the heel. Bursitis, An inflamed bursa is a small irritated sack of fluid at the back of the heel. Other types of heel pain include soft tissue growths, Haglunds deformity (bone enlargement at the back of the heel), bruises or stress fractures and possible nerve entrapment.
Diagnosis
A biomechanical exam by your podiatrist will help reveal these abnormalities and in turn resolve the cause of plantar fasciitis. By addressing this cause, the patient can be offered a podiatric long-term solution to his problem.
Non Surgical Treatment
Recommended treatments, heel Spurs: cushioning for the heel is of little value. Your chiropodist/podiatrist may initially apply padding and strapping to alter the direction of stretch of the ligament. This is often successful at reducing the tenderness in the short term. Your chiropodist/podiatrist may suggest a course of deep heat therapy to stimulate the healing processes, allowing damage to respond and heal faster. In the long term, your chiropodist/podiatrist may prescribe special insoles (orthoses) to help the feet to function more effectively, thereby reducing strain on the ligaments and making any recurrence less likely. If pain from heel spurs continues, you may be referred to your GP who can prescribe an oral non-steroidal anti-inflammatory. Alternatively, localised hydrocortisone injection treatment may be given by your GP or an appropriate chiropodist/podiatrist. If pain persists, surgery may be considered. Heel Bursitis: in most cases, attention to the cause of any rubbing, and appropriate padding and strapping by your chiropodist/podiatrist will allow the inflammation to settle. If infection is present, your chiropodist/podiatrist will refer you to your GP for antibiotics. Heel Bumps: adjustments to footwear is often enough to make them comfortable. A leather heel counter and wearing boots may help. However, if pain persists, surgery may be necessary.
Surgical Treatment
Extracorporeal shockwave therapy (EST) is a fairly new type of non-invasive treatment. Non-invasive means it does not involve making cuts into your body. EST involves using a device to deliver high-energy soundwaves into your heel. The soundwaves can sometimes cause pain, so a local anaesthetic may be used to numb your heel. It is claimed that EST works in two ways. It is thought to have a "numbing" effect on the nerves that transmit pain signals to your brain, help stimulate and speed up the healing process. However, these claims have not yet been definitively proven. The National Institute for Health and Care Excellence (NICE) has issued guidance about the use of EST for treating plantar fasciitis. NICE states there are no concerns over the safety of EST, but there are uncertainties about how effective the procedure is for treating heel pain. Some studies have reported that EST is more effective than surgery and other non-surgical treatments, while other studies found the procedure to be no better than a placebo (sham treatment).
no foot pain
Prevention

Before you get out of bed in the morning, and then periodically throughout the day, do the following exercises to increase flexibility and ease pain. Slowly flex your foot and toes to stretch the tissue on the bottom of your sore foot. Hold the stretch for 10 counts. Relax and repeat. Do gentle ankle rolls to keep the tissues around the ankle and on the back of the heel flexible. Sit on the edge of your bed and roll your foot back and forth over a tennis ball.
Leg Length Discrepancy Shoe Inserts
Overview
Limb-length discrepancies or differences are conditions that result in limbs that are unequal in length or that exhibit other anomalies. The conditions occur when bones or joints in the arms or legs are abnormal or become damaged. Providers might refer to these conditions as limb-length discrepancies, limb differences or limb-length conditions.
Causes
From an anatomical stand point, the LLD could have been from hereditary, broken bones, diseases and joint replacements. Functional LLD can be from over pronating, knee deformities, tight calves and hamstrings, weak IT band, curvature in the spine and many other such muscular/skeletal issues.
Symptoms
In addition to the distinctive walk of a person with leg length discrepancy, over time, other deformities may be noted, which help compensate for the condition. Toe walking on the short side to decrease the swaying during gait. The foot will supinate (high arch) on the shorter side. The foot will pronate (flattening of the arch) on the longer side. Excessive pronation leads to hypermobility and instability, resulting in metatarsus primus varus and associated unilateral juvenile hallux valgus (bunion) deformity.
Diagnosis
On standing examination one iliac crest may be higher/lower than the other. However a physiotherapist, osteopath or chiropractor will examine the LLD in prone or supine position and measure it, confirming the diagnosis of structural (or functional) LLD. The LLD should be measured using bony fixed points. X-Ray should be taken in a standing position. The osteopath, physiotherapist or chiropractor will look at femoral head & acetabulum, knee joints, ankle joints.
Non Surgical Treatment
A personalized approach to leg length discrepancy treatment works best for each patient. Your child's doctor will consider many factors when deciding on a course of treatment for this condition. Such factors can include your child's age, extent of the leg length discrepancy, medical history, how your child tolerates certain treatments and procedures, your child's health and prognosis, growth rate, and parental preferences. There is no cookie cutter treatment for each child, or even each centimeter of leg difference. Once all of these factors have been carefully considered, your child's physician will come up with an appropriate course of care. In situations of a very small leg length discrepancy, no treatment, only periodic medical evaluation, may be necessary.

height increase medicine
Surgical Treatment
Surgical lengthening of the shorter extremity (upper or lower) is another treatment option. The bone is lengthened by surgically applying an external fixator to the extremity in the operating room. The external fixator, a scaffold-like frame, is connected to the bone with wires, pins or both. A small crack is made in the bone and tension is created by the frame when it is "distracted" by the patient or family member who turns an affixed dial several times daily. The lengthening process begins approximately five to ten days after surgery. The bone may lengthen one millimeter per day, or approximately one inch per month. Lengthening may be slower in adults overall and in a bone that has been previously injured or undergone prior surgery. Bones in patients with potential blood vessel abnormalities (i.e., cigarette smokers) may also lengthen more slowly. The external fixator is worn until the bone is strong enough to support the patient safely, approximately three months per inch of lengthening. This may vary, however, due to factors such as age, health, smoking, participation in rehabilitation, etc. Risks of this procedure include infection at the site of wires and pins, stiffness of the adjacent joints and slight over or under correction of the bone?s length. Lengthening requires regular follow up visits to the physician?s office, meticulous hygiene of the pins and wires, diligent adjustment of the frame several times daily and rehabilitation as prescribed by your physician.
Limb-length discrepancies or differences are conditions that result in limbs that are unequal in length or that exhibit other anomalies. The conditions occur when bones or joints in the arms or legs are abnormal or become damaged. Providers might refer to these conditions as limb-length discrepancies, limb differences or limb-length conditions.

Causes
From an anatomical stand point, the LLD could have been from hereditary, broken bones, diseases and joint replacements. Functional LLD can be from over pronating, knee deformities, tight calves and hamstrings, weak IT band, curvature in the spine and many other such muscular/skeletal issues.
Symptoms
In addition to the distinctive walk of a person with leg length discrepancy, over time, other deformities may be noted, which help compensate for the condition. Toe walking on the short side to decrease the swaying during gait. The foot will supinate (high arch) on the shorter side. The foot will pronate (flattening of the arch) on the longer side. Excessive pronation leads to hypermobility and instability, resulting in metatarsus primus varus and associated unilateral juvenile hallux valgus (bunion) deformity.
Diagnosis
On standing examination one iliac crest may be higher/lower than the other. However a physiotherapist, osteopath or chiropractor will examine the LLD in prone or supine position and measure it, confirming the diagnosis of structural (or functional) LLD. The LLD should be measured using bony fixed points. X-Ray should be taken in a standing position. The osteopath, physiotherapist or chiropractor will look at femoral head & acetabulum, knee joints, ankle joints.
Non Surgical Treatment
A personalized approach to leg length discrepancy treatment works best for each patient. Your child's doctor will consider many factors when deciding on a course of treatment for this condition. Such factors can include your child's age, extent of the leg length discrepancy, medical history, how your child tolerates certain treatments and procedures, your child's health and prognosis, growth rate, and parental preferences. There is no cookie cutter treatment for each child, or even each centimeter of leg difference. Once all of these factors have been carefully considered, your child's physician will come up with an appropriate course of care. In situations of a very small leg length discrepancy, no treatment, only periodic medical evaluation, may be necessary.

height increase medicine
Surgical Treatment
Surgical lengthening of the shorter extremity (upper or lower) is another treatment option. The bone is lengthened by surgically applying an external fixator to the extremity in the operating room. The external fixator, a scaffold-like frame, is connected to the bone with wires, pins or both. A small crack is made in the bone and tension is created by the frame when it is "distracted" by the patient or family member who turns an affixed dial several times daily. The lengthening process begins approximately five to ten days after surgery. The bone may lengthen one millimeter per day, or approximately one inch per month. Lengthening may be slower in adults overall and in a bone that has been previously injured or undergone prior surgery. Bones in patients with potential blood vessel abnormalities (i.e., cigarette smokers) may also lengthen more slowly. The external fixator is worn until the bone is strong enough to support the patient safely, approximately three months per inch of lengthening. This may vary, however, due to factors such as age, health, smoking, participation in rehabilitation, etc. Risks of this procedure include infection at the site of wires and pins, stiffness of the adjacent joints and slight over or under correction of the bone?s length. Lengthening requires regular follow up visits to the physician?s office, meticulous hygiene of the pins and wires, diligent adjustment of the frame several times daily and rehabilitation as prescribed by your physician.
What Is Mortons Neuroma
Overview
 Morton's neuroma is a painful condition that affects the ball of your foot, most commonly the area between your third and fourth toes. Morton's neuroma may feel as if you are standing on a pebble in your shoe or on a fold in your sock. Morton's neuroma involves a thickening of the tissue around one of the nerves leading to your toes. This can cause a sharp, burning pain in the ball of your foot. Your toes also may sting, burn or feel numb. High-heeled shoes have been linked to the development of Morton's neuroma. Many people experience relief by switching to lower heeled shoes with wider toe boxes. Sometimes corticosteroid injections or surgery may be necessary.
Morton's neuroma is a painful condition that affects the ball of your foot, most commonly the area between your third and fourth toes. Morton's neuroma may feel as if you are standing on a pebble in your shoe or on a fold in your sock. Morton's neuroma involves a thickening of the tissue around one of the nerves leading to your toes. This can cause a sharp, burning pain in the ball of your foot. Your toes also may sting, burn or feel numb. High-heeled shoes have been linked to the development of Morton's neuroma. Many people experience relief by switching to lower heeled shoes with wider toe boxes. Sometimes corticosteroid injections or surgery may be necessary.
Causes
A Morton?s Neuroma are a result of complex biomechanical changes that occur in your feet. There are a number of theories as to the exact cause of the scarring and thickening, but it basically boils down to overload of the tissue structure. The body lays down scar tissue to try to protect the overloaded structure. Tight-fitting shoes may exacerbate a Morton?s Neuroma. Shoes such as high heels and shoes with tight toe boxes (eg womens fashion shoes and cowboy boots) are particularly damaging to the toes. These shoes have a sloping foot bed and a narrow toe box. The slope causes the front of the foot to bear your weight. The angle of the toe box then squeezes your toes together. Footwear is not the only cause of a Morton?s Neuroma. Injuries to the foot can also be a factor in developing the condition by changing your foot biomechanics. Poor foot arch control leading to flat feet or foot overpronation does make you biomechanically susceptible to a neuroma.
Symptoms
People with Morton's neuroma usually complain of pain that can start in the ball of the foot and shoot into the affected toes. However, some people just have toe pain. There may also be burning and tingling of the toes. The symptoms are usually felt up the sides of the space between two toes. For example, if the nerve between the third and fourth long bones (metatarsals) of the right foot is affected, the symptoms will usually be felt up the right-hand side of the fourth toe and up the left-hand side of the third toe. Some people describe the pain that they feel as being like walking on a stone or a marble. Symptoms can be made worse if you wear high-heeled shoes. The pain is relieved by taking your shoe off, resting your foot and massaging the area. You may also experience some numbness between the affected toes. Your affected toes may also appear to be spread apart, which doctors refer to as the 'V sign'. The symptoms can vary and may come and go over a number of years. For example, some people may experience two attacks of pain in a week and then nothing for a year. Others may have regular and persistent (chronic) pain.
Diagnosis
You might first seek advice from your family doctor about your foot pain. He or she may refer you to a doctor or surgeon who specializes in foot disorders. Before your appointment, you may want to write a list of answers to the following questions. When did your symptoms begin? Did your symptoms begin gradually or suddenly? What type of footwear do you wear for work? Do you participate in sports? If so, what types in particular? What medications and supplements do you take regularly? Your doctor may ask some of the following questions. Is the pain worse in certain pairs of shoes? Does any type of activity ease the pain or worsen it? Are you having pain in any other part of your body?
Non Surgical Treatment
In most cases, initial treatment for this condition consists of padding and taping to disperse weight away from the neuroma. If the patient has flatfeet, an arch support is incorporated into footwear. The patient is instructed to wear shoes with wide toe boxes and avoid shoes with high heels. An injection of local anesthetic to relieve pain and a corticosteroid to reduce inflammation may be administered. The patient is advised to return in a week or 2 to monitor progress. If the pain has been relieved, the neuroma is probably small and caused by the structure of the patient's foot and the type of shoes the patient wears. It can be relieved by a custom-fitted orthotic that helps maintain the foot in a better position. Another type of therapy that may be used is alcohol sclerosing injections. In this treatment, the doctor injects a small amount of alcohol in the area of the neuroma area to help harden (sclerose) the nerve and relieve the pain. Injections are given every 7-10 days and, in many cases, 4-7 injections are needed for maximum relief. Please ask your physician for more information regarding this type of treatment.
Surgical Treatment
The ultimate success of a Morton?s neuroma treated surgically is somewhat unclear. This is likely due to the idea that in most instances a ?Morton?s neuroma? is actually more than just an isolated nerve problem but rather consitutes a metatarsalgia where other structures (such a as the MTP joints) are also problematic, not just the nerve. Therefore, addressing the nerve as well as the other components of a metatarsalgia may offer a better chance of surgical success. However, like many conditions in foot and ankle, it is ideal if this condition can be managed without surgery.
 Morton's neuroma is a painful condition that affects the ball of your foot, most commonly the area between your third and fourth toes. Morton's neuroma may feel as if you are standing on a pebble in your shoe or on a fold in your sock. Morton's neuroma involves a thickening of the tissue around one of the nerves leading to your toes. This can cause a sharp, burning pain in the ball of your foot. Your toes also may sting, burn or feel numb. High-heeled shoes have been linked to the development of Morton's neuroma. Many people experience relief by switching to lower heeled shoes with wider toe boxes. Sometimes corticosteroid injections or surgery may be necessary.
Morton's neuroma is a painful condition that affects the ball of your foot, most commonly the area between your third and fourth toes. Morton's neuroma may feel as if you are standing on a pebble in your shoe or on a fold in your sock. Morton's neuroma involves a thickening of the tissue around one of the nerves leading to your toes. This can cause a sharp, burning pain in the ball of your foot. Your toes also may sting, burn or feel numb. High-heeled shoes have been linked to the development of Morton's neuroma. Many people experience relief by switching to lower heeled shoes with wider toe boxes. Sometimes corticosteroid injections or surgery may be necessary.Causes
A Morton?s Neuroma are a result of complex biomechanical changes that occur in your feet. There are a number of theories as to the exact cause of the scarring and thickening, but it basically boils down to overload of the tissue structure. The body lays down scar tissue to try to protect the overloaded structure. Tight-fitting shoes may exacerbate a Morton?s Neuroma. Shoes such as high heels and shoes with tight toe boxes (eg womens fashion shoes and cowboy boots) are particularly damaging to the toes. These shoes have a sloping foot bed and a narrow toe box. The slope causes the front of the foot to bear your weight. The angle of the toe box then squeezes your toes together. Footwear is not the only cause of a Morton?s Neuroma. Injuries to the foot can also be a factor in developing the condition by changing your foot biomechanics. Poor foot arch control leading to flat feet or foot overpronation does make you biomechanically susceptible to a neuroma.
Symptoms
People with Morton's neuroma usually complain of pain that can start in the ball of the foot and shoot into the affected toes. However, some people just have toe pain. There may also be burning and tingling of the toes. The symptoms are usually felt up the sides of the space between two toes. For example, if the nerve between the third and fourth long bones (metatarsals) of the right foot is affected, the symptoms will usually be felt up the right-hand side of the fourth toe and up the left-hand side of the third toe. Some people describe the pain that they feel as being like walking on a stone or a marble. Symptoms can be made worse if you wear high-heeled shoes. The pain is relieved by taking your shoe off, resting your foot and massaging the area. You may also experience some numbness between the affected toes. Your affected toes may also appear to be spread apart, which doctors refer to as the 'V sign'. The symptoms can vary and may come and go over a number of years. For example, some people may experience two attacks of pain in a week and then nothing for a year. Others may have regular and persistent (chronic) pain.
Diagnosis
You might first seek advice from your family doctor about your foot pain. He or she may refer you to a doctor or surgeon who specializes in foot disorders. Before your appointment, you may want to write a list of answers to the following questions. When did your symptoms begin? Did your symptoms begin gradually or suddenly? What type of footwear do you wear for work? Do you participate in sports? If so, what types in particular? What medications and supplements do you take regularly? Your doctor may ask some of the following questions. Is the pain worse in certain pairs of shoes? Does any type of activity ease the pain or worsen it? Are you having pain in any other part of your body?
Non Surgical Treatment
In most cases, initial treatment for this condition consists of padding and taping to disperse weight away from the neuroma. If the patient has flatfeet, an arch support is incorporated into footwear. The patient is instructed to wear shoes with wide toe boxes and avoid shoes with high heels. An injection of local anesthetic to relieve pain and a corticosteroid to reduce inflammation may be administered. The patient is advised to return in a week or 2 to monitor progress. If the pain has been relieved, the neuroma is probably small and caused by the structure of the patient's foot and the type of shoes the patient wears. It can be relieved by a custom-fitted orthotic that helps maintain the foot in a better position. Another type of therapy that may be used is alcohol sclerosing injections. In this treatment, the doctor injects a small amount of alcohol in the area of the neuroma area to help harden (sclerose) the nerve and relieve the pain. Injections are given every 7-10 days and, in many cases, 4-7 injections are needed for maximum relief. Please ask your physician for more information regarding this type of treatment.

Surgical Treatment
The ultimate success of a Morton?s neuroma treated surgically is somewhat unclear. This is likely due to the idea that in most instances a ?Morton?s neuroma? is actually more than just an isolated nerve problem but rather consitutes a metatarsalgia where other structures (such a as the MTP joints) are also problematic, not just the nerve. Therefore, addressing the nerve as well as the other components of a metatarsalgia may offer a better chance of surgical success. However, like many conditions in foot and ankle, it is ideal if this condition can be managed without surgery.
Shoe Lifts The Podiatrists Option For Leg Length Imbalances
There are actually two different kinds of leg length discrepancies, congenital and acquired. Congenital implies you are born with it. One leg is structurally shorter in comparison to the other. As a result of developmental stages of aging, the human brain picks up on the step pattern and identifies some variance. Our bodies typically adapts by dipping one shoulder over to the "short" side. A difference of under a quarter inch is not very excessive, doesn't need Shoe Lifts to compensate and usually won't have a profound effect over a lifetime.

Leg length inequality goes mainly undiscovered on a daily basis, however this condition is very easily fixed, and can eliminate a number of instances of back discomfort.
Therapy for leg length inequality commonly consists of Shoe Lifts. These are typically low cost, often priced at under twenty dollars, compared to a custom orthotic of $200 or even more. Differences over a quarter inch can take their toll on the spine and should probably be compensated for with a heel lift. In some cases, the shortage can be so extreme that it requires a full lift to both the heel and sole of the shoe.
Lumbar pain is the most common condition afflicting men and women today. Around 80 million men and women are afflicted by back pain at some point in their life. It's a problem that costs businesses huge amounts of money yearly due to time lost and production. Innovative and superior treatment methods are constantly sought after in the hope of lowering economical influence this condition causes.

People from all corners of the earth experience foot ache as a result of leg length discrepancy. In a lot of these cases Shoe Lifts can be of very helpful. The lifts are capable of decreasing any discomfort in the feet. Shoe Lifts are recommended by countless qualified orthopaedic orthopedists.
In order to support the human body in a nicely balanced manner, the feet have got a critical job to play. Inspite of that, it can be the most overlooked area of the human body. Many people have flat-feet meaning there is unequal force placed on the feet. This causes other parts of the body including knees, ankles and backs to be affected too. Shoe Lifts make sure that ideal posture and balance are restored.

Leg length inequality goes mainly undiscovered on a daily basis, however this condition is very easily fixed, and can eliminate a number of instances of back discomfort.
Therapy for leg length inequality commonly consists of Shoe Lifts. These are typically low cost, often priced at under twenty dollars, compared to a custom orthotic of $200 or even more. Differences over a quarter inch can take their toll on the spine and should probably be compensated for with a heel lift. In some cases, the shortage can be so extreme that it requires a full lift to both the heel and sole of the shoe.
Lumbar pain is the most common condition afflicting men and women today. Around 80 million men and women are afflicted by back pain at some point in their life. It's a problem that costs businesses huge amounts of money yearly due to time lost and production. Innovative and superior treatment methods are constantly sought after in the hope of lowering economical influence this condition causes.

People from all corners of the earth experience foot ache as a result of leg length discrepancy. In a lot of these cases Shoe Lifts can be of very helpful. The lifts are capable of decreasing any discomfort in the feet. Shoe Lifts are recommended by countless qualified orthopaedic orthopedists.
In order to support the human body in a nicely balanced manner, the feet have got a critical job to play. Inspite of that, it can be the most overlooked area of the human body. Many people have flat-feet meaning there is unequal force placed on the feet. This causes other parts of the body including knees, ankles and backs to be affected too. Shoe Lifts make sure that ideal posture and balance are restored.
Hammertoes Treatment Options
 Overview
Overview
There are two different types. Flexible Hammer toes. These are less serious because they can be diagnosed and treated while still in the developmental stage. They are called flexible hammertoes because they are still moveable at the joint. Rigid Hammertoes. This variety is more developed and more serious than the flexible condition. Rigid hammertoes can be seen in patients with severe arthritis, for example, or in patients who wait too long to seek professional treatment. The tendons in a rigid hammertoe have become tight, and the joint misaligned and immobile, making surgery the usual course of treatment.
Causes
Essentially, hammertoes are caused by an abnormal interworking of the bones, muscles, ligaments and tendons that comprise your feet. When muscles fail to work in a balanced manner, the toe joints can bend to form the hammertoe shape. If they remain in this position for an extended period, the muscles and tendons supporting them tighten and remain in that position. A common factor in development of hammertoe is wearing shoes that squeeze the toes or high heels that jam the toes into the front of the shoe. Most likely due to these factors, hammertoe occurs much more frequently in women than in men.
 Symptoms
Symptoms
The symptoms of hammertoe are progressive, meaning that they get worse over time. Hammertoe causes the middle joint on the second, third, fourth, or fifth toes to bend. The affected toe may be painful or irritated, especially when you wear shoes. Areas of thickened skin (corns) may develop between, on top of, or at the end of your toes. Thickened skin (calluses) may also appear on the bottom of your toe or the ball of your foot. It may be difficult to find a pair of shoes that is comfortable to wear.
Diagnosis
Most health care professionals can diagnose hammertoe simply by examining your toes and feet. X-rays of the feet are not needed to diagnose hammertoe, but they may be useful to look for signs of some types of arthritis (such as rheumatoid arthritis) or other disorders that can cause hammertoe. If the deformed toe is very painful, your doctor may recommend that you have a fluid sample withdrawn from the joint with a needle so the fluid can be checked for signs of infection or gout (arthritis from crystal deposits).
Non Surgical Treatment
A person with hammer toes will be asked to practice some exercises for their toes to regain average structure and movement. The exercises usually involve stretching and strengthening their toes. The person may attempt to pick things up off the floor using only their toes. They may also stretch their toes on a regular basis by hand to ease them into straightening out. Another example of a physical exercise specifically for a person's toes involves crumpling a towel with the toes. The towel can lie underneath the person's feet and the person can use their toes to scrunch up the towel as they perform simple tasks such as reading a book or watching television.
Surgical Treatment
If a person's toes have become very inflexible and unresponsive to non-invasive means of treatment and if open sores have developed as a result of constant friction, they may receive orthopaedic surgery to correct the deformity. The operation is quick and is commonly performed as an out-patient procedure. The doctor administers a local anesthetic into the person's foot to numb the site of the operation. The person may remain Hammer toes conscious as the surgeon performs the procedure. A sedative might also be administered to help calm the person if they are too anxious.
 Prevention
Prevention
In addition to wearing proper shoes and socks, walking often and properly can prevent foot injury and pain. The head should be erect, the back straight, and the arms relaxed and swinging freely at the side. Step out on the heel, move forward with the weight on the outside of the foot, and complete the step by pushing off the big toe. Exercises specifically for the toe and feet are easy to perform and help strengthen them and keep them flexible. Helpful exercises include the following. Raise and curl the toes 10 times, holding each position for a count of five. Put a rubber band around both big toes and pull the feet away from each other. Count to five. Repeat 10 times. Pick up a towel with the toes. Repeat five times. Pump the foot up and down to stretch the calf and shin muscles. Perform for 2 or 3 minutes.